Canada Gazette, Part I, Volume 151, Number 24: Regulations Amending the Food and Drug Regulations (Opioids)
June 17, 2017
Statutory authority
Food and Drugs Act
Sponsoring department
Department of Health
REGULATORY IMPACT ANALYSIS STATEMENT
(This statement is not part of the Regulations.)
Executive summary
Issues: The potential for harm associated with opioid drugs and the growing related public health crisis is the subject of increasing concern for Canadians and other levels of government in Canada. Health Canada has identified the need for strengthened post-market oversight of opioids to help monitor and mitigate their risks, and the need for patients to receive additional, clear information about the safe use of opioids and the risks associated with their use.
Description: The proposed amendments to the Food and Drugs Regulations would expressly permit the Minister of Health (the Minister) to add or amend terms and conditions to an authorization for the sale of an opioid. This authority could then be used by the Minister to compel an opioid authorization holder to develop and implement a risk management plan to appropriately monitor, quantify, characterize and mitigate the risks associated with post-market use of these products. The proposed amendments would also require that a patient information handout and warning sticker accompany prescription opioids at the time of sale.
Cost-benefit statement: The costs of this proposal are associated with the requirement to print and provide the patient information handout and to apply a warning sticker to opioid containers. These costs have been estimated at $76,522,000 over a 10-year period when discounted at 7% and are expected to be borne primarily by pharmacies.
These costs would be offset by a number of qualitative benefits, including patients receiving key information that is expected to increase their awareness of the risks associated with opioids and encourage safer use of these drugs. The benefits associated with the ability to impose terms and conditions on opioid authorizations arise from stronger post-market oversight of opioids in Canada, including the ability to require, for example, the development and implementation of risk management plans for opioids. Such plans would be expected to result in measures to mitigate risks identified with these products and better protect the health and safety of Canadians.
“One-for-One” Rule and small business lens: The “One-for-One” Rule does not apply to this proposal, as it is not expected to increase the administrative burden on businesses.
The small business lens applies, as over three quarters of pharmacies are considered small businesses. The requirement to provide a patient information handout and apply a warning sticker whenever opioids are dispensed is expected to increase costs for small businesses by $1,075 annually. To minimize the burden on small businesses, a flexible regulatory option was identified: the patient information handout has been designed to be printed in black and white. This aspect of the proposal would also have a six-month coming-into-force provision to facilitate compliance with the new requirements. This flexible regulatory option would reduce compliance costs for small businesses by $36,862,000 over 10 years.
Domestic and international coordination and cooperation: The proposed amendments would enhance Health Canada's regulatory alignment with the United States and the European Union.
Background
Opioid crisis and federal response
Opioids offer effective pain relief for many patients. Examples of opioids include oxycodone, morphine, hydromorphone, fentanyl, and codeine. The strength of opioid medications varies greatly, and nearly all are available by prescription only, the exception being products that contain low doses of codeine.
Opioids pose potential harms due to the safety risks associated with this class of drugs, including their association with dependency, addiction, overdose and death. Physical dependence occurs with daily use of opioids, and can make it difficult to stop taking these medicines. Furthermore, people who are physically dependent on opioids may experience withdrawal symptoms if they stop using the drug abruptly. Long-term use of opioids can lead to development of tolerance, making higher doses necessary to maintain the intensity of their effects. Opioid overdose can lead to death and is more likely at higher doses. Taking an opioid with alcohol or other sedating drugs increases the risk of overdose and death.
Before the 1990s, prescription opioids were primarily used for palliative care, cancer pain, or post-surgical pain. In the late 1990s, rates of opioid prescribing grew rapidly. Canadians are the second highest per capita consumers of prescription opioids in the world, and their use of prescription opioids increased by 203% between 2000 and 2010. (see footnote 1)
Increased rates of use of both prescription and illicit opioids, increased rates of addiction, and increased rates of overdose deaths are a serious and growing public health and safety crisis across Canada, attracting significant public concern. A 2016 study by the Canadian Institute for Health Information and the Canadian Centre on Substance Abuse reports that between 2007–2008 and 2014–2015, the rate of hospitalizations due to opioid poisoning increased by more than 30%. (see footnote 2) In Ontario, 10.6% of individuals seeking addiction treatment in 2005–2006 were seeking treatment for addiction to prescription opioids. By 2010–2011, this had increased to 18.6%. (see footnote 3)
A significant element of the federal response to the growing public health crisis due to opioids was announced by the Minister on June 17, 2016. Provincial jurisdictions are also taking action to address the opioid crisis. The Government of British Columbia declared a public health emergency in early 2016, and announced the development of an opioid task force shortly thereafter. Other provinces, including Alberta, Nova Scotia, and Ontario, have also launched opioid strategies. On November 19, 2016, the Minister and Ontario's Minister of Health and Long-Term Care co-hosted a multi-stakeholder Opioid Conference and Summit, resulting in the Joint Statement of Action to Address the Opioid Crisis (Joint Statement of Action) describing planned actions on opioids by the Government of Canada, nine provincial and territorial governments, and over 30 health organizations. (see footnote 4)
Two of the proposed federal initiatives to address the opioid crisis would require amendments to the Food and Drug Regulations (the Regulations) to be implemented. The first is a requirement for risk management plans (RMPs) for opioids. The second is a requirement for a warning sticker and patient information handout to be provided with all prescription opioids at time of dispensing.
Health Canada (the Department) convened the external Scientific Advisory Panel on Opioids in November 2016 to provide expert advice from scientific, medical, and patient perspectives on these requirements. Specifically, the panel provided recommendations on the content of the proposed warning sticker and patient information handout as well as the types of risk monitoring and minimization activities that could be included in RMPs for opioids. (see footnote 5)
Post-market oversight
(i) Terms and conditions
The Minister is currently permitted to impose and amend terms and conditions on authorizations for medical devices, establishment licences, and blood collected for transfusion or use in the manufacture of a drug for human use at the time of authorization or post-market, but not on authorizations for the sale of drugs. At present, Health Canada places conditions on some drug authorizations under the Notice of Compliance with Conditions (NOC/c) policy, but these terms and conditions are not legally enforceable. With the passage of the Protecting Canadians from Unsafe Drugs Act (Vanessa's Law), which amended the Food and Drugs Act in 2014, regulations can be made in respect of terms and conditions on authorizations issued for therapeutic products, including drugs.
(ii) Risk management plans
The decision to approve a drug for sale in Canada is based on it having a satisfactory balance of benefits and risks if the drug is used within the conditions specified in the product labelling. This decision is based on the information available at the time of approval. However, knowledge related to the safety profile of the drug can change over time through expanded use once the product is on the market. An RMP is a living document developed by the sponsor or authorization holder of a drug. It consists of a set of activities and interventions designed to monitor, quantify, characterize and mitigate risks relating to the product. It may also include a means for assessing the effectiveness of any interventions. Ideally, an RMP is updated throughout the product's life cycle to reflect new and emerging knowledge about the product's safety profile, based upon discussion and agreement between the Department and the authorization holder.
An RMP generally has the following three elements:
- Safety specification: a summary of the known important safety information about the drug, and gaps in knowledge (uncertainties).
- Pharmacovigilance plan: a set of risk-monitoring activities undertaken to better characterize known or potential safety concerns. These can include routine activities such as reporting of adverse drug reactions, and additional activities such as post-market safety and drug utilization studies.
- Risk minimization measures: a set of activities to minimize any identified or potential safety risks. These can include routine activities such as warnings on the label, and additional activities such as training or the development of additional educational material. The information generated from the risk-monitoring activities of the pharmacovigilance plan is used as the basis to develop and adjust the risk minimization measures.
Departmental guidance (see footnote 6) requests RMPs for all new drugs coming onto the market. Although an RMP is not explicitly listed as a submission requirement in the Regulations, it contains key information on how the product's sponsor intends to monitor, quantify, characterize and mitigate the risks associated with the product once it has entered the market. In certain circumstances, the Department will request that an authorization holder voluntarily provide an RMP for a drug that is already on the market, including for
- a marketed drug for which a serious safety issue has been identified;
- a previously acceptable RMP that has undergone significant changes (for example to reflect new knowledge about the product);
- drugs new to a class for which a serious or potentially serious safety risk has been identified for another member of the class; or
- when it is determined that an RMP is required for the establishment of an adequate risk minimization framework.
The RMPs for opioids that have been reviewed by the Department to date have included risk minimization measures that have been voluntarily implemented by the authorization holders. These measures have focused on risk education and communication and include, for example, guides for patients, caregivers and prescribers, educational material, requirement for field representatives to highlight the potential for problematic use when contacting prescribers, “dear health care provider” professional communications, and health care professional education through accredited programs.
The majority of opioids currently available on the Canadian market do not have RMPs because they were authorized for sale prior to the Department implementing RMP reviews.
Warning stickers and patient information
Provisions in the Regulations require certain information to appear on the labels of drugs at the time they are dispensed. For example, when a prescription drug is dispensed, the label must contain the name of the drug, the potency of the drug, the name of the drug's manufacturer, and suitable directions for use. Typically, pharmacists are responsible for complying with these labelling requirements, since they are generally responsible for dispensing drugs to patients at the point of sale. Certain practitioners, for example doctors or nurse practitioners, may also dispense and sell drugs to patients, depending on the province or territory in which they practice; however, data is not available regarding the extent to which this occurs.
Currently, patients sometimes receive additional information handouts about prescription opioids when they are dispensed; however, handouts can vary from pharmacy to pharmacy and the information tends to focus on how to take the drug (i.e. with or without food), how often, and its possible side effects. Stickers for prescription drugs are typically applied to the container at the discretion of the pharmacist at the time of dispensing, and can vary from pharmacy to pharmacy. Stickers can be obtained from pharmacy wholesale distributors. In addition, it is becoming increasingly common for pharmacy software vendors to incorporate stickers into their standard prescription label sets. It is at the pharmacist's discretion to select a sticker or patient information sheet to be distributed with a dispensed drug. While there are a few exceptions, these materials are largely unregulated at the provincial level.
Issues
Need for strengthened post-market oversight of opioids
Given the potential for harm associated with opioids, and the growing public health crisis due in part to their use, strengthened post-market oversight of opioids in the Canadian market is needed to help monitor, quantify, characterize, and mitigate the risks of these drugs.
Reliable and comprehensive data on the risks and potential for problematic use of opioids in the post-approval phase in Canada is lacking because the Minister does not have a means to require this type of information from authorization holders. Furthermore, there is currently no means by which the Minister can require authorization holders to conduct risk minimization activities to mitigate risks that have been identified with opioids following their entry into the Canadian market.
The Minister needs to be able to impose these types of requirements on opioid authorization holders so that risks associated with these drugs can be identified and managed as effectively as possible and the health and safety of Canadians can be better protected.
Need for patients to be better informed about the risks of opioids
Patients need to receive consistent and relevant information about the safe use and the risks of opioids, particularly the potential for dependency, addiction and overdose (including death), beyond what is already listed on the prescription label and provided to them at the time of dispensing. This information needs to be concise and easy to understand, and contain the most important key messages to help patients better understand the risks of opioid use.
Objectives
The objectives of the proposed regulatory amendments are to
- Strengthen the post-market oversight of prescription opioids, allowing for earlier identification of risks and earlier and more effective interventions, by authorizing the Minister to impose terms and conditions on opioid authorization holders; and
- Better inform Canadian patients about the safe use of opioids and their associated risks, via a mandatory warning sticker and patient information handout for prescribed opioids at the time of dispensing.
The proposed regulatory amendments would act on the Minister's commitment to take action on this public health and safety crisis by allowing the fulfillment of two announced initiatives.
Description
1. Implement terms and conditions to strengthen post-market oversight of opioids
The proposed amendments would expressly permit the Minister to add or amend legally enforceable terms and conditions to an authorization for the sale of an opioid.
The Minister could then use this authority to require opioid authorization holders to develop and submit to the Department an RMP and to undertake the activities set out in it, in order to help manage the uncertainties or mitigate the harms of the opioid on the market. In addition to existing on-market opioids, the Minister could also use this new authority to impose terms and conditions requiring RMPs on the authorizations for new opioids following their entry to the market.
Further, the Minister could also use this authority to impose or amend any other type of term and condition on an opioid should the need arise.
This would be the first regulatory proposal to make use of the authority to make regulations regarding terms and conditions that was brought into force with the enactment of the Protecting Canadians from Unsafe Drugs Act (Vanessa's Law), which amended the Food and Drugs Act in 2014.
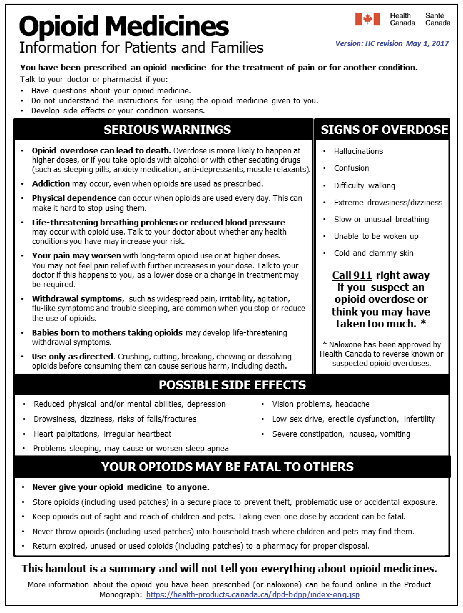
2. Mandatory patient information handout and warning sticker
The proposed amendments would require a pharmacist or practitioner selling a prescription opioid to affix the Health Canada–approved warning sticker to the prescription opioid bottle, container or package, and to provide the Health Canada–approved patient information handout to the patient every time an opioid is sold.
The required patient information handout and warning sticker would be set out in a separate administrative document that would be incorporated by reference into the Food and Drug Regulations. A copy of this document is attached in Appendix 1. This would permit the Department to update the content of the sticker and patient information handout as needed to prevent injury to health. This document would be administered by the Department and published on its website. Stakeholders would be notified of any subsequent changes to this document and provided with an opportunity to comment, as per Health Canada's policy on modifications to documents incorporated by reference. (see footnote 7)
The warning sticker and patient information handout have been developed by Health Canada based on input from the external Scientific Advisory Panel on Opioids. While the panel provided valuable input, final responsibility for the content and format of the sticker and handout remains with Health Canada. Therefore, following the panel, internal focus groups with subject-matter experts were held to ensure the content is free of major gaps in serious opioid warnings and precautions, is consistent with the recently updated Canadian Product Monographs for approved opioids, and is written in language that is as clear and plain as possible. The sticker also underwent patient user testing to assess the effectiveness and clarity of the content and design.
The warning sticker would warn patients about the risks of opioid dependence, addiction and overdose. The patient information handout would provide broader information on the safe use of opioids and their associated risks.
3. Scope of proposed amendments
The aforementioned proposed requirements would be limited to prescription opioids included on the List of Opioids (the List), which would be incorporated by reference into the Regulations. A copy of the List is attached in Appendix 2. The List would include products by active ingredient so that authorization holders, health care practitioners, and the public would know with certainty to which products these provisions are meant to apply. The List would be administered by the Department and published on its website. Stakeholders would be notified of any subsequent changes to the List and provided with an opportunity to comment, as per Health Canada's policy on modifications to documents incorporated by reference.
4. Other minor amendments
Section C.01.005 and subsection C.01.014(1) of the Regulations would also be amended to better reflect modern drafting terminology and to address inconsistencies between the English and French versions of those provisions.
5. Coming into force
The proposed regulatory amendments in respect of the terms and conditions to increase post-market oversight of opioids would come into force on the day on which the Regulations are registered. Health Canada will notify the World Trade Organization (WTO) of this timeline, as per its obligations under the Agreement on Technical Barriers to Trade.
The proposed regulatory amendments in respect of the patient information handout and warning sticker would come into force six months after the day on which the Regulations are registered. This would provide stakeholders time to effectively implement the new requirements.
Regulatory and non-regulatory options considered
1. Strengthening post-market oversight of opioids
The Department considered the alternative regulatory option of placing a prohibition on sale to prevent an opioid authorization holder from selling an opioid unless they had provided Health Canada with an RMP. This regulatory option would only serve to ensure that RMPs were developed and provided to Health Canada. Under this option, Health Canada could not compel an authorization holder to carry out the activities set out within the RMP. It is critical that the Department have a legal mechanism for enforcing the post-market commitments set out within an RMP in order for the RMP to have true value; therefore, this option was not adopted. Instead, the terms and conditions authority was selected as the appropriate regulatory tool because the Minister could use this authority to make legally enforceable the wide variety of activities needed in an RMP to identify and minimize post-market risks.
2. Mandatory patient information handout and warning sticker
(i) Labelling requirement for manufacturers
The Department considered the alternative regulatory option of amending the Regulations such that the manufacturer would be required to include the warning sticker and patient information handout as part of the drug's label. However, this option would not address the need for this information to accompany the prescription opioid at the point of sale when the medication is dispensed to the patient. Like most medications, prescription opioids are generally not dispensed to the patient in the manufacturer's original packaging, but rather they are repackaged by the pharmacist or practitioner into a smaller container. The pharmacist or practitioner, as the party who dispenses the medication to the patient, and not the manufacturer, is best placed to affix the warning sticker to the final container that is provided to the patient and to ensure that the medication is accompanied by an information handout when dispensed. This option was therefore not adopted.
(ii) Voluntary labelling by pharmacists and practitioners
The Department considered the non-regulatory option of voluntary labelling by pharmacists and practitioners. However, at present, pharmacists and practitioners decide which labels to affix to the container of a prescribed opioid drug and which handouts to provide to patients; therefore, the information the patient receives can vary. Because this information is critical to the health and safety of Canadians, Health Canada is of the view that the same information needs to be consistently provided to all patients receiving a prescription opioid at the time of dispensing. The proposed amendment would allow for consistency of delivery of information such that Canadians in all provinces and territories would receive the same Health Canada–approved warnings about the risks associated with opioid use.
Benefits and costs
The stakeholder groups that would be directly impacted by this regulatory proposal include Canadian patients, pharmacists in retail pharmacies, practitioners who dispense and sell opioids to patients, and opioid authorization holders.
Benefits
Informing patients about the risks of opioids
In order for patients to be better informed about the safe use and associated risks of opioids, their opioid prescriptions would be accompanied by a Health Canada–approved warning sticker and patient information handout with standardized easy-to-understand information about the safe use and significant risks associated with opioids, such as dependence, addiction, and overdose. The application of a warning sticker on the container of prescription opioids would serve as an additional reminder to be cautious when taking opioids, due to their likelihood to cause physical dependence, their addictive nature and the risk of overdose and death.
The benefits of patients receiving information about the safe use and risks associated with opioids have been assessed qualitatively. A literature review has not revealed any studies quantifying the effect of labels and information handouts for pharmaceuticals on patient behaviour.
The proposed requirements are expected to increase patient awareness of the risks associated with opioids and encourage safer use of these drugs. It is important to note that modifying the labels of drugs to communicate risks is a standard approach that Health Canada uses. The sticker and handout, which are additional labels, are expected to lead to patients having a better understanding of the risks to their health, and the health of others, of the opioids that have been prescribed to them, and what they can do to mitigate these risks. It is expected that this knowledge would influence patients' behaviour, leading to safer use of prescribed opioids, and a reduced incidence of actual and potential harms from use. For example, having easy-to-understand information at hand about the signs of opioid overdose is expected to increase awareness of these symptoms among patients and their families and lead to patients having conversations with pharmacists and their physicians as well as allow earlier intervention if overdose occurs.
In addition, these requirements are expected to help prevent opioid exposure in children and others. A study by the Institute for Clinical Evaluative Sciences and The Hospital for Sick Children found that children of women prescribed an opioid painkiller face a risk that is nearly 2.5 times higher of being hospitalized for opioid overdose than children whose mothers do not receive these drugs. The study concluded that measures should be taken to mitigate the risk of opioid-related harm to children, including emphasizing to parents the importance of proper disposal and keeping opioid drugs away from young children. (see footnote 8) In a similar vein, an American study of pediatric exposure to opioids concluded that greater efforts are needed to prevent opioid exposure to children of all ages. (see footnote 9) Consistent with these conclusions, the proposed patient information handout would include information about the importance of keeping opioid medication in a safe place away from children and of not disposing of it where it could be found by children in order to avoid the risk of theft or accidental exposure. This information is expected to lead to patients taking greater care in storing and disposing of their opioids, thus reducing the risk of theft or accidental or intentional consumption by children and others.
Strengthening post-market oversight of opioids via terms and conditions on opioid authorizations
The ability to impose terms and conditions on an opioid authorization would not result in any directly measurable benefits. Rather, benefits would occur if the Minister carries out her intention to impose terms and conditions on opioid authorization holders, for example, by requiring them to develop and submit an RMP to the Department and carry out the activities specified within it. While a literature review has not revealed any studies quantifying the benefits of RMPs, the imposition of terms and conditions requiring their development and implementation would result in activities to monitor, quantify, characterize and mitigate the risks to Canadians associated with post-market use of opioids. Because they are intended to mitigate risks to Canadians associated with opioids, the Department expects that such measures would result in a reduction of opioid-related harms and associated health care costs to the Canadian population.
Costs
Distribution of patient information handout and application of warning sticker
The proposal would require prescription opioids to be dispensed with a warning sticker and patient handout containing information on safe use and associated risks. The present value costs of these requirements are estimated at $76,522,000 over 10 years. Because data is not available regarding the extent to which non-pharmacists (i.e. practitioners) dispense opioid drugs, it is assumed that these costs would primarily be borne by pharmacists.
These costs were estimated using the following assumptions:
- Pharmacists earn an hourly wage of $50.00 per hour.
- The requirement to affix a sticker to the containers of dispensed opioids would result in a negligible increase in the time it takes for a pharmacist to dispense an opioid because warning stickers are often affixed to containers of dispensed medications.
- Warning stickers can be bought in bulk at a cost of $5 for 1 000 stickers.
- Providing patients with an opioid-specific Health Canada–approved patient information handout would take a pharmacist, on average, half a minute.
- Printing the information handout would cost approximately 2.5¢ per page.
- 21.7 million opioid products were dispensed in 2014. Prior to that, opioid dispensing was increasing, and the increase in dispensing has been extrapolated to 2027.
- The warning sticker and information handout would have to be provided every time an opioid product is dispensed.
Terms and conditions on opioid authorizations
This aspect of the proposal would amend the Regulations to permit the Minister to impose terms and conditions on opioid authorization holders. Although the proposed amendments would not impose any direct costs on industry, there would be costs if the Minister carries out her intention to impose terms and conditions on opioid authorization holders, requiring them to develop and submit an RMP to the Department, and undertake the activities set out in it. The Department surveyed industry in January 2017 regarding RMPs. The costs of developing and implementing an RMP for opioids, as reported by respondents, ranged from $1.2 million to $16.0 million.
The full cost-benefit analysis is available upon request.
| Stakeholder | Base Year | Final Year | Total (Present Value) |
Annualized Average | |
|---|---|---|---|---|---|
| Quantified impacts (in Can$, 2017 price level / constant dollars) Costs |
|||||
| Purchasing warning stickers | Pharmacists and practitioners | $55,000 | $135,000 | $857,000 | $117,000 |
| Printing and providing informational handouts | Pharmacists and practitioners | $4,889,000 | $11,931,000 | $75,665,000 | $10,363,000 |
| Total costs | $76,522,000 | $10,480,000 | |||
| Qualitative impacts Benefits |
|||||
|
|||||
“One-for-One” Rule
The “One-for-One” Rule does not apply to this proposal, as the regulatory amendments are not expected to increase the administrative burden on businesses.
Small business lens
The proposed amendment to require that a warning sticker and a patient information handout be provided to patients would impact small business by virtue of the fact that pharmacists would be responsible for affixing the warning sticker to the prescription opioid container, and for providing the patient information handout, every time an opioid is dispensed. Roughly 78% of pharmacies in Canada have annual revenues between $30,000 and $5 million, thus meeting the definition of small business.
The proposed requirements are understandable in everyday language and the List of Opioids would provide clarity as to which products would be required to be dispensed with the warning sticker and a patient information handout. There is a clear connection between the requirement to affix the warning sticker and provide the handout and the objective of the Regulations to provide patients with understandable and consistent information about the safe use of opioid drugs and their associated risks.
The Department conducted initial outreach with pharmacy stakeholders in March 2017 to raise awareness of the regulatory proposal and begin dialogue on implementation. During this session, the Department heard that not all pharmacies have colour printers.
A number of efforts have been made to accommodate the needs of small businesses. For example, to minimize the impact on pharmacies that do not have access to high-speed internet, the proposed warning sticker and patient information handout have been designed to minimize use of Internet bandwidth (no high-resolution graphics, black and white text for the patient information handout).
The proposed amendment to allow terms and conditions to be attached to opioid authorizations would affect drug manufacturing companies but would not impact small businesses.
Regulatory flexibility analysis statement
The initial regulatory option was an immediate coming into force for the mandatory warning sticker and patient information handout, with the handout being in colour. The flexible regulatory option identified was to have a six-month coming-into-force provision for the mandatory warning sticker and patient information handout, with the handout being in black and white. The flexible option would reduce compliance costs for small business by $36,862,000 over 10 years. The flexible option was chosen for the proposed amendments.
| Initial Option | Flexible Option | |||
|---|---|---|---|---|
| Short description |
|
|
||
| Number of small businesses impacted | 7 605 | 7 605 | ||
| Annualized Average ($) | Present Value (see footnote a) ($) | Annualized Average ($) | Present Value (see footnote b) ($) | |
| Compliance costs (itemize if appropriate) | 15,274,000 | 113,384,000 | 10,480,000 | 76,522,000 |
| Administrative costs (itemize if appropriate) | 0 | 0 | 0 | 0 |
| Total costs (all small businesses) | 15,274,000 | 113,384,000 | 10,480,000 | 76,522,000 |
| Total cost per small business | 1,567 | 11,629 | 1,075 | 7,848 |
| Risk considerations | Small businesses would not have sufficient time to prepare to comply with the Regulations. | This would delay patients receiving important information on the risks of opioids. | ||
Note: Costs have been estimated using the Standard Cost Model. Detailed calculations are available upon request.
Consultation
When Vanessa's Law was being considered by Parliament in 2013–14, Health Canada heard from industry stakeholders in respect of the regulation-making authority to impose terms and conditions on authorizations. Industry stakeholders indicated that they wanted to be certain that any future terms and conditions imposed upon authorizations would be applied in a manner that is fair. The Department affirms that administrative law principles set out in “Amendments to the Food and Drugs Act: Guide to New Authorities” will apply to the Minister's use of the proposed terms and conditions authority such that, unless circumstances warrant otherwise, an authorization holder would have sufficient notice of the Minister's intention to impose terms and conditions on an authorization so that the authorization holder would have an opportunity to be heard.
The Minister announced her intention to bring forward proposals to require a warning sticker, a patient information handout, and risk management plans for opioids in June 2016, and again in November 2016 in the Joint Statement of Action to Address the Opioid Crisis. The Joint Statement of Action is a combined commitment on the part of nine provincial and territorial governments (British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Northwest Territories, Nova Scotia, Ontario, Prince Edward Island, and Saskatchewan) and over 30 health stakeholders, including pharmacy stakeholders, to act on the opioid crisis. As a result, the actions outlined within it are broadly supported by these governments and organizations. In a statement to the Standing Committee on Health in October 2016, the Canadian Pharmacists Association indicated that it supports the Government's announcement that it will proceed with regulatory changes that require opioids to carry a warning sticker and come with a patient information handout. (see footnote 10)
In November 2016, a Scientific Advisory Panel on Opioids provided expert advice on the content of the proposed warning sticker and patient information handout, as well as on potential risk monitoring and risk minimization activities that could be requested of authorization holders for inclusion in their RMPs.
Given that the Department envisions that the authority to add terms and conditions could be used to require RMPs, a survey focusing on RMPs was sent to drug industry associations in January 2017. Suggestions from stakeholders to reduce the potential burden of RMPs included collaboration among companies; application of a risk-based approach when determining the extent of monitoring and risk mitigation activities; and the development of common RMPs specific to groups of opioids with similar characteristics rather than RMPs specific to each product. It was also noted that some aspects of risk mitigation are beyond the manufacturer's control; therefore, stakeholders beyond industry should be included in the consultation and implementation processes. One stakeholder noted that requiring extensive RMPs may limit the number of products available on the market due to cost concerns. These responses have been taken into consideration in the development of a draft guidance document regarding RMPs for opioids.
As part of its routine engagement activities with stakeholders, the Department took the opportunity to brief two pharmacy stakeholder organizations in March 2017 to raise awareness of the proposed amendments, seek input, and begin discussion on implementation considerations. Some concerns were raised regarding the need for a regulatory approach to achieve the objective of having dispensed opioids be accompanied by a warning sticker and patient information handout. Stakeholders noted that further consultation will be needed to fully identify and address implementation issues, for example updating pharmacy dispensing software. Stakeholders will have a more formal opportunity to provide comments during the consultation process following the publication of the proposed amendments in the Canada Gazette, Part I. Further targeted discussions with stakeholders will also take place before and after publication in the Canada Gazette, Part I, to inform the implementation plan.
The proposed warning sticker reflects the outcome of patient user testing on several versions of the proposed warning sticker conducted by the Department in March 2017.
Regulatory cooperation
While the primary purpose of this regulatory proposal is to inform patients about the safe use of opioids and mitigate their associated risks, the proposed amendments would also bring Canada into closer alignment with other jurisdictions, including the United States and the European Union, as these jurisdictions already have in place a number of regulatory tools to increase the post-market oversight of all drugs, including opioids. These include tools to compel authorization holders to provide the regulator with RMPs.
Companies are required to submit an RMP to the European Medicines Agency when they apply for an authorization of their medicinal product. In addition, for nationally authorized medicinal products in the European Union, any national regulatory authority can request an RMP whenever there is a concern about a risk that affects the benefit-risk balance of a medicine. When justified by risk, a national regulatory authority can also specify a date for submission of the next RMP as a condition of the marketing authorization in exceptional cases.
Similarly, the U.S. Food and Drug Administration (FDA) has had authority since 2007 to require sponsors and authorization holders to develop and comply with Risk Evaluation and Mitigation Strategies (REMS), which are similar to the risk minimization portion of an RMP. It also has the ability to place additional post-market commitments on authorizations for drugs, including opioids. These commitments are used, for example, to gather additional information about a drug's safety, efficacy or optimal use. The U.S. FDA has used this authority to require, for example, a REMS program for extended release opioids, (see footnote 11) and a prospective, observational study designed to quantify the serious risks of problematic use and addiction associated with long-term use of opioid analgesics for management of chronic pain among patients prescribed extended release opioid analgesics. (see footnote 12)
With respect to labelling, in September 2013 and March 2016, the U.S. FDA introduced safety labelling changes for prescription opioid products to include additional information on their risks. New requirements include a new warning about the serious risks of problematic use, abuse, addiction, overdose and death. Similarly, in December 2014, the United Kingdom Medicines and Healthcare Products Regulatory Agency issued guidance concerning additional detailed warning statements expected to be included on the carton and patient information leaflet for the opioid fentanyl.
Rationale
The proposed amendments are necessary to protect Canadians from the serious and growing public health threat presented by the opioid crisis. Providing the Minister with an ability to impose enforceable terms and conditions for prescription opioids will significantly improve Health Canada's post-market oversight of these drugs so that their risks can be better identified and mitigated. Requiring a warning sticker and patient information handout for prescription opioids at time of sale will provide key information to patients about the safe use of opioids and their associated risks of dependency, addiction and potentially fatal overdose.
In the absence of the proposed amendments, the Minister would not have appropriate authority to require post-market activities aimed at monitoring, quantifying and minimizing risks to Canadians posed by prescription opioids. Furthermore, the Department could not be assured that patients would be provided with key information about the safe use and the risks associated with these drugs.
Imposing terms and conditions and requiring a warning sticker and patient information handout for prescription opioids is proportionate to the degree of risk these products pose to the population, particularly in light of the public health crisis associated with increased rates of problematic use, addiction, and overdose deaths, and is in line with how the risks of these drugs are addressed in other jurisdictions.
Implementation, enforcement and service standards
Once the Regulations Amending the Food and Drug Regulations (Opioids) [the proposed Regulations] are in force, the Minister could place terms and conditions on authorizations for opioids to require and enforce RMPs. Implementation would follow a phased approach by beginning with the highest priority opioids as determined by the Department, informed by feedback from the Scientific Advisory Panel on Opioids. The panel agreed that all opioids carry the risk of harm but suggested that the Department prioritize those opioids that are currently implicated in the majority of opioid-related harms in Canada.
A guidance document would set out expectations for RMP content and set out the process by which the Minister would impose, add, or amend terms and conditions on an opioid authorization. Administrative law principles of procedural fairness would be built into the process, in keeping with the “Amendments to the Food and Drugs Act: Guide to New Authorities.” (see footnote 13) Draft guidance will be made available on the Health Canada website.
In addition, once the proposed Regulations are in force, pharmacists and practitioners selling a drug on the List of Opioids would have to affix the Health Canada–approved warning sticker to the prescription opioid's bottle, container or package and provide the Health Canada–approved patient information handout with the drug. The warning sticker and patient information handout would be set out in a document to be incorporated by reference into the Food and Drug Regulations. The graphic for the warning sticker and patient information handout would be available on Health Canada's website. The approach to implementation would be determined following consultation with key pharmacy and other stakeholders. Health Canada would also revise the Labelling Guidance for Industry to include a section specific to the warning sticker and handout.
Compliance and enforcement of the proposed Regulations would be in accordance with a risk-based approach, aligned with departmental policies, including compliance promotion activities.
All terms and conditions would be enforceable under section 21.7 of the Food and Drugs Act. This means that if an authorization holder were not to respond to requests from the Department to comply with the terms and conditions imposed, the Department would consider pursuing compliance and enforcement measures, as per its Compliance and Enforcement Policy, (see footnote 14) and court action, such as injunction or prosecution, could result.
Other existing compliance and enforcement related regulatory provisions, such as stop-sale, label change, or cancellation of authorization, would continue to apply to opioids just as they apply to all marketed drugs.
Contact
Bruno Rodrigue
Policy, Planning and International Affairs Directorate
Health Products and Food Branch
Health Canada
Holland Cross, Suite 14
11 Holland Avenue
Ottawa, Ontario
K1A 0K9
AL: 3000A
Email: LRM_MLR_consultations@hc-sc.gc.ca
APPENDIX 1: Draft Information for Patients Concerning Opioids
(Warning Sticker and Patient Information Handout)
Part A: Opioid Warning Sticker
Part B: Opioid Patient Information Handout
APPENDIX 2: List of Opioids
| Drugs intended for human use containing any of the following active ingredients | Including (but not limited to) |
Qualifier |
|---|---|---|
| Buprenorphine | Buprenorphine Hydrochloride | |
| Butorphanol | Butorphanol Tartrate | |
| Codeine | Codeine Phosphate | Except for those products referred to in subsection 36(1) of the Narcotic Control Regulations. |
| Fentanyl | Fentanyl Citrate | |
| Hydrocodone | Hydrocodone Bitartrate | |
| Hydromorphone | Hydromorphone Hydrochloride | |
| Meperidine | Meperidine Hydrochloride | |
| Methadone | Methadone Hydrochloride | |
| Morphine | Morphine Hydrochloride; Morphine Sulfate | |
| Normethadone | Normethadone Hydrochloride | |
| Opium | Opium and Belladonna | |
| Oxycodone | Oxycodone Hydrochloride | |
| Oxymorphone | Oxymorphone Hydrochloride | |
| Pentazocine | Pentazocine Hydrochloride; Pentazocine Lactate | |
| Tapentadol | Tapentadol Hydrochloride | |
| Tramadol | Tramadol Hydrochloride |
| Drugs intended for human use containing any of the following active ingredients | Including (but not limited to) | Qualifier |
|---|---|---|
| Buprenorphine | Buprenorphine Hydrochloride | |
| Butorphanol | Butorphanol Tartrate | |
| Codeine | Codeine Phosphate | Except for those products referred to in subsection 36(1) of the Narcotic Control Regulations. |
| Fentanyl | Fentanyl Citrate | |
| Hydrocodone | Hydrocodone Bitartrate | |
| Hydromorphone | Hydromorphone Hydrochloride | |
| Meperidine | Meperidine Hydrochloride | |
| Methadone | Methadone Hydrochloride | |
| Morphine | Morphine Hydrochloride; Morphine Sulfate | |
| Normethadone | Normethadone Hydrochloride | |
| Opium | Opium and Belladonna | |
| Oxycodone | Oxycodone Hydrochloride | |
| Oxymorphone | Oxymorphone Hydrochloride | |
| Pentazocine | Pentazocine Hydrochloride; Pentazocine Lactate | |
| Tapentadol | Tapentadol Hydrochloride | |
| Tramadol | Tramadol Hydrochloride |
Small Business Lens Checklist
1. Name of the sponsoring regulatory organization:
Health Canada
2. Title of the regulatory proposal:
Regulations Amending the Food and Drug Regulations — Labelling and RMPs for Opioids
3. Is the checklist submitted with a RIAS for the Canada Gazette, Part I or Part II?
☑ Canada Gazette, Part I ☐ Canada Gazette, Part II
| I | Communication and transparency | Yes | No | N/A |
|---|---|---|---|---|
| 1. | Are the proposed Regulations or requirements easily understandable in everyday language? | ☑ | ☐ | ☐ |
| 2. | Is there a clear connection between the requirements and the purpose (or intent) of the proposed Regulations? | ☑ | ☐ | ☐ |
| 3. | Will there be an implementation plan that includes communications and compliance promotion activities, that informs small business of a regulatory change and guides them on how to comply with it (e.g. information sessions, sample assessments, toolkits, websites)? | ☑ | ☐ | ☐ |
| 4. | If new forms, reports or processes are introduced, are they consistent in appearance and format with other relevant government forms, reports or processes? | ☐ | ☐ | ☑ |
| There are no new government forms, reports or processes. | ||||
| II | Simplification and streamlining | Yes | No | N/A |
| 1. | Will streamlined processes be put in place (e.g. through BizPaL, Canada Border Services Agency single window) to collect information from small businesses where possible? | ☐ | ☐ | ☑ |
| No information will be collected. | ||||
| 2. | Have opportunities to align with other obligations imposed on business by federal, provincial, municipal or international or multinational regulatory bodies been assessed? | ☑ | ☐ | ☐ |
| 3. | Has the impact of the proposed Regulations on international or interprovincial trade been assessed? | ☐ | ☐ | ☑ |
| Trade will not be affected by this proposal. | ||||
| 4. | If the data or information, other than personal information, required to comply with the proposed Regulations is already collected by another department or jurisdiction, will this information be obtained from that department or jurisdiction instead of requesting the same information from small businesses or other stakeholders? (The collection, retention, use, disclosure and disposal of personal information are all subject to the requirements of the Privacy Act. Any questions with respect to compliance with the Privacy Act should be referred to the department's or agency's ATIP office or legal services unit.) | ☐ | ☐ | ☑ |
| No data will be collected. | ||||
| 5. | Will forms be pre-populated with information or data already available to the department to reduce the time and cost necessary to complete them? (Example: When a business completes an online application for a licence, upon entering an identifier or a name, the system pre-populates the application with the applicant's personal particulars such as contact information, date, etc. when that information is already available to the department.) | ☐ | ☐ | ☑ |
| There are no forms to be filled out. | ||||
| 6. | Will electronic reporting and data collection be used, including electronic validation and confirmation of receipt of reports where appropriate? | ☐ | ☐ | ☑ |
| There will be no reporting or data collection. | ||||
| 7. | Will reporting, if required by the proposed Regulations, be aligned with generally used business processes or international standards if possible? | ☐ | ☐ | ☑ |
| There will be no reporting required. | ||||
| 8. | If additional forms are required, can they be streamlined with existing forms that must be completed for other government information requirements? | ☐ | ☐ | ☑ |
| There are no forms to be filled out. | ||||
| III | Implementation, compliance and service standards | Yes | No | N/A |
| 1. | Has consideration been given to small businesses in remote areas, with special consideration to those that do not have access to high-speed (broadband) Internet? | ☑ | ☐ | ☐ |
| 2. | If regulatory authorizations (e.g. licences, permits or certifications) are introduced, will service standards addressing timeliness of decision making be developed that are inclusive of complaints about poor service? | ☐ | ☐ | ☑ |
| No regulatory authorizations will be introduced. | ||||
| 3. | Is there a clearly identified contact point or help desk for small businesses and other stakeholders? | ☑ | ☐ | ☐ |
| IV | Regulatory flexibility analysis | Yes | No | N/A |
|---|---|---|---|---|
| 1. | Does the RIAS identify at least one flexible option that has lower compliance or administrative costs for small businesses in the small business lens section? Examples of flexible options to minimize costs are as follows:
|
☑ | ☐ | ☐ |
| 2. | Does the RIAS include, as part of the Regulatory Flexibility Analysis Statement, quantified and monetized compliance and administrative costs for small businesses associated with the initial option assessed, as well as the flexible, lower-cost option? | ☑ | ☐ | ☐ |
| 3. | Does the RIAS include, as part of the Regulatory Flexibility Analysis Statement, a consideration of the risks associated with the flexible option? (Minimizing administrative or compliance costs for small business cannot be at the expense of greater health, security or safety or create environmental risks for Canadians.) | ☑ | ☐ | ☐ |
| 4. | Does the RIAS include a summary of feedback provided by small business during consultations? | ☑ | ☐ | ☐ |
| V | Reverse onus | Yes | No | N/A |
| 1. | If the recommended option is not the lower-cost option for small business in terms of administrative or compliance costs, is a reasonable justification provided in the RIAS? | ☐ | ☐ | ☑ |
| The lower cost option was chosen. | ||||
PROPOSED REGULATORY TEXT
Notice is given that the Governor in Council, pursuant to section 30 (see footnote c) of the Food and Drugs Act (see footnote d), proposes to make the annexed Regulations Amending the Food and Drug Regulations (Opioids).
Interested persons may make representations concerning the proposed Regulations within 75 days after the date of publication of this notice. All such representations must cite the Canada Gazette, Part I, and the date of publication of this notice, and be addressed to Bruno Rodrigue, Office of Legislative and Regulatory Modernization, Policy, Planning and International Affairs Directorate, Health Products and Food Branch, Department of Health, Holland Cross, Tower A, Ground Floor, Suite 14, 11 Holland Avenue, Address Locator: 3000A, Ottawa, Ontario K1A 0K9 (email: LRM_MLR_consultations@hc-sc.gc.ca).
Ottawa, June 8, 2017
Jurica Čapkun
Assistant Clerk of the Privy Council
Regulations Amending the Food and Drug Regulations (Opioids)
Amendments
1 Section C.01.005 of the Food and Drug Regulations (see footnote 15) is replaced by the following:
C.01.005 (1) The principal display panel of both the inner label and outer label of a drug in dosage form shall show the drug identification number assigned for that drug, preceded by the expression “Drug Identification Number” or “Drogue : identification numérique”, or both, or the abbreviation “DIN”.
(2) Subsection (1) does not apply to
- (a) a drug in dosage form that is compounded by a pharmacist under a prescription or by a practitioner; or
- (b) a drug in dosage form that is sold under a prescription if the following information appears on the drug's label:
- (i) the drug's proper name, common name or brand name,
- (ii) the drug's potency, and
- (iii) the name of the drug's manufacturer.
(3) In this section and in sections C.01.005.1 and C.01.014, drug in dosage form means a drug in a form in which it is ready for use by the consumer without requiring any further manufacturing.
C.01.005.1 (1) No pharmacist or practitioner shall sell a Class A opioid — including one that is compounded by a pharmacist under a prescription or by a practitioner — unless
- (a) the drug's package has applied to it a warning sticker that meets the specifications set out in the source document; and
- (b) the drug is accompanied by a patient information sheet that meets the specifications set out in the source document.
(2) The following definitions apply in subsection (1):
Class A opioid means a drug in dosage form set out in Part A of the List of Opioids, published by the Government of Canada on its website, as amended from time to time. (opioïde de catégorie A)
source document means the document entitled Information for Patients Concerning Opioids, published by the Government of Canada on its website, as amended from time to time. (document source)
2 Subsection C.01.014(1) of the Regulations is replaced by the following:
C.01.014 (1) No manufacturer shall sell a drug in dosage form unless a drug identification number has been assigned for that drug and the assignment of the number has not been cancelled under section C.01.014.6.
3 The Regulations are amended by adding the following after section C.01.014.2:
C.01.014.21 (1) The Minister may, at any time, impose terms and conditions on a drug identification number assigned for a Class B opioid, or amend those terms and conditions.
(2) The Minister shall notify, in writing, the manufacturer to whom a document was issued under subsection C.01.014.2(1) that sets out the drug identification number of any terms and conditions imposed on the drug identification number and of any amendment of those terms and conditions.
(3) In subsection (1), Class B opioid means a drug set out in Part B of the List of Opioids, published by the Government of Canada on its website, as amended from time to time.
Coming into Force
4 (1) These Regulations, except section 3, come into force on the day that, in the sixth month after the month in which they are registered, has the same calendar number as the day on which they are registered, or, if that sixth month has no day with that number, the last day of that sixth month.
(2) Section 3 comes into force on the day on which these Regulations are registered.
[24-1-o]